President Trump has signed the One Big Beautiful Bill Act into law, and I want to walk you through the healthcare provisions that will directly impact millions of Americans. Title VII focuses on finance, with Subtitle B specifically addressing health programs. Given the widespread concern about these changes, I will provide a comprehensive breakdown of what this means for you and your family.
Overview of Title VII’s Healthcare Framework
Title VII restructures major aspects of American healthcare financing, targeting Medicaid, Medicare, health insurance tax credits, and rural healthcare infrastructure. The legislation introduces significant changes across five main areas, each with different implementation timelines spanning from 2026 through 2034.
Subchapter A: Reducing Fraud and Improving Enrollment Processes
The Act implements several measures designed to prevent fraudulent enrollment and improve system efficiency. Two major enrollment rule implementations are suspended until September 2034, providing states additional time to adapt their systems.
The legislation establishes a national system to prevent individuals from enrolling in Medicaid programs in multiple states simultaneously. Beginning October 2029, states must submit enrollment information monthly to this federal system, including social security numbers and other identifying information. This system aims to eliminate duplicate coverage and reduce administrative costs.
For deceased individuals, states must now conduct quarterly reviews of the Death Master File to identify and disenroll deceased beneficiaries from Medicaid. This requirement begins January 2027 and extends to healthcare providers, who must also be screened against death records during enrollment and quarterly thereafter starting January 2028.
The Act modifies how eligibility redeterminations work for certain Medicaid expansion populations. Beginning January 2027, adults covered under Medicaid expansion must undergo eligibility reviews every six months instead of annually, potentially affecting millions of beneficiaries who will need to provide documentation more frequently.
Additionally, the legislation revises home equity limits for long-term care eligibility. The maximum home value exemption increases to $1,000,000 for non-agricultural properties, while agricultural properties maintain more flexible standards based on state election.
Subchapter B: Preventing Wasteful Spending
This section implements cost-reduction measures that directly affect beneficiary services. The Act places a moratorium on nursing home staffing standards until September 2034, suspending requirements for minimum nurse staffing levels that were scheduled to take effect.
Retroactive coverage under Medicaid faces significant restrictions. Currently, Medicaid can cover medical expenses up to three months before application. The new law reduces this to one month for expansion populations and two months for traditional Medicaid beneficiaries, beginning with applications made after December 2026.
The legislation specifically targets Planned Parenthood and similar organizations through funding restrictions. Organizations meeting specific criteria related to abortion services and receiving over $800,000 in annual Medicaid funding face a one-year funding prohibition beginning with the Act’s enactment.
Subchapter C: Stopping Abusive Financing Practices
The Act phases out the enhanced federal matching rate for Medicaid expansion, requiring states to begin expansion before January 2026 to maintain current funding levels. States that expanded Medicaid after this date will not receive the enhanced 90% federal matching rate.
Provider tax regulations become more restrictive, with different rules applying to expansion and non-expansion states. Expansion states face gradually decreasing limits on provider taxes, dropping from 5.5% in 2028 to 3.5% by 2032. Non-expansion states maintain their current tax levels if enacted before the law’s passage, but face 0% limits for new taxes.
State-directed payments under Medicaid managed care face significant limitations. Expansion states can only pay up to 100% of Medicare rates, while non-expansion states can pay up to 110% of Medicare rates. Existing arrangements receive a gradual phase-down beginning in 2028, with 10 percentage point annual reductions until reaching the new limits.
The legislation requires budget neutrality for all Medicaid demonstration projects beginning January 2027. The Chief Actuary must certify that projects will not increase federal spending compared to what would occur without the demonstration.
Subchapter D: Increasing Personal Accountability
Perhaps the most significant change for beneficiaries involves new work requirements for Medicaid expansion populations. Beginning no later than January 2027, able-bodied adults aged 19-64 in the Medicaid expansion population must demonstrate community engagement through work, education, training, or community service for at least 80 hours monthly.
Extensive exemptions apply to vulnerable populations, including pregnant women, caregivers of children under 13 or disabled individuals, people with disabilities, veterans with total disability ratings, individuals with substance use disorders, and those in treatment programs. States can also provide temporary exemptions for hardship situations.
Non-compliance results in disenrollment after a 30-day notice period, though individuals can reapply once they meet requirements. States must conduct outreach and provide verification assistance, with implementation flexibility through December 2028 for states demonstrating good faith efforts.
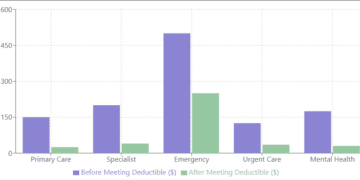
The Act also introduces new cost-sharing requirements for expansion populations with incomes above the poverty line, beginning October 2028. While premiums are prohibited, states must impose copayments and deductibles up to $35 per service, with total family cost-sharing capped at 5% of income quarterly.
Subchapter E: Expanding Access to Care
Despite restrictions in other areas, the Act expands access to home and community-based services. Beginning July 2028, states can obtain waivers to provide these services to individuals who do not require institutional-level care, potentially serving more people in community settings.
States must demonstrate that these expanded services will not increase wait times for those requiring institutional-level care and that per-capita costs remain below institutional care expenses. This provision aims to serve more people while controlling overall program costs.
Medicare Changes
The Act restricts Medicare eligibility to citizens, lawful permanent residents, Cuban and Haitian entrants, and individuals residing under Compacts of Free Association. Current beneficiaries not meeting these criteria face termination 18 months after enactment, following a review process by the Social Security Administration.
Medicare physician payments receive a temporary 2.5% increase for 2026, providing short-term relief to healthcare providers. The drug price negotiation program expands its orphan drug exclusion, potentially affecting medication costs for rare diseases.
Health Insurance Tax Credit Modifications
Premium tax credits through healthcare marketplaces face new restrictions. Beginning in 2027, only citizens, lawful permanent residents, Cuban and Haitian entrants, and individuals under Compacts of Free Association qualify for these credits.
The Act eliminates income-based limits on premium tax credit recapture, meaning individuals who receive advance payments but end up ineligible must repay the full amount regardless of income. Enhanced verification requirements take effect in 2028, requiring exchanges to verify eligibility before enrollment and maintain comprehensive documentation.
Special enrollment periods face restrictions, with premium tax credits unavailable for coverage obtained during income-based special enrollment periods not connected to qualifying life events.
Rural Healthcare Investment
The Act establishes a Rural Health Transformation Program providing $50 billion over five years (2026-2030) to the 50 states. States must submit detailed rural health transformation plans addressing access, outcomes, technology adoption, workforce development, and financial sustainability.
Funding supports evidence-based interventions, technology solutions, workforce recruitment, information technology advances, and innovative care models. This represents a significant federal investment in rural healthcare infrastructure and services.
Implementation Timeline and Considerations
These changes implement on varying schedules, with some beginning immediately and others phased in through 2034. The staggered timeline allows states and beneficiaries time to adapt, though significant preparation will be required.
Healthcare providers, state agencies, and beneficiaries should begin preparing now for these changes. The work requirements, eligibility restrictions, and funding modifications will require careful planning and potentially difficult transitions for affected individuals and organizations.
The Act represents a fundamental shift toward more restrictive eligibility criteria, increased beneficiary responsibility, and enhanced program integrity measures, while simultaneously investing in rural healthcare infrastructure and expanding certain community-based services. Understanding these changes will be crucial for navigating the evolving healthcare landscape in the coming years.
For more content, check out the following:
- Understanding Title I of the One Big Beautiful Bill Act: What These Agricultural and Nutrition Changes Mean for You
- Breaking Down the One Big Beautiful Bill Act: What Title II Means for Defense and National Security
- Breaking Down the One Big Beautiful Bill Act: Title III and Its Impact on Financial Oversight
- Breaking Down Title IV of the One Big Beautiful Bill Act: What It Means for Commerce, Science, and Transportation
- Understanding Title V of the One Big Beautiful Bill Act: Energy and Natural Resources
- Understanding Title VI of the One Big Beautiful Bill Act: What It Means for Environmental Programs and You